Sarcomas are a very rare form of cancer in the field of tumor diseases. They can appear anywhere in the body. In gynecology, sarcomas are even rarer, as they form a subfamily of soft tissue sarcomas as part of the female genital tract. Since they initially cause little pain, sarcomas are often dismissed as harmless swellings. The rarity is due to the fact that the treating doctor has significantly less literature and guidelines to fall back on than is the case with common types of cancer such as breast or lung cancer.
A sarcoma is a malignant tumor that develops in soft tissue (muscle, fat and connective tissue). The number of new sarcoma cases in Germany is estimated at around 5,000 per year. These most commonly occur on the extremities (arms and legs). However, sarcomas can also develop in the female genital organs such as the womb (uterus), ovaries (ovaries), vagina (vagina) or vulva. In this case, doctors usually refer to this as gynecological sarcomas. Compared to classic gynecological cancers such as ovarian or cervical cancer, gynecological sarcomas make up only a small proportion of gynecological malignant diseases. It is estimated that only a maximum of 2% of all gynecological cancers are gynecological sarcomas.
Soft tissue sarcomas can occur at any age. However, they occur more frequently in childhood and adolescence as well as in adulthood between the ages of 45 and 55. Gynecological sarcomas such as B. a leiomyosarcoma of the uterus or a sarcoma of the ovary, almost never occur in childhood, but are a disease of adult women.
Not every gynecologic sarcoma is the same
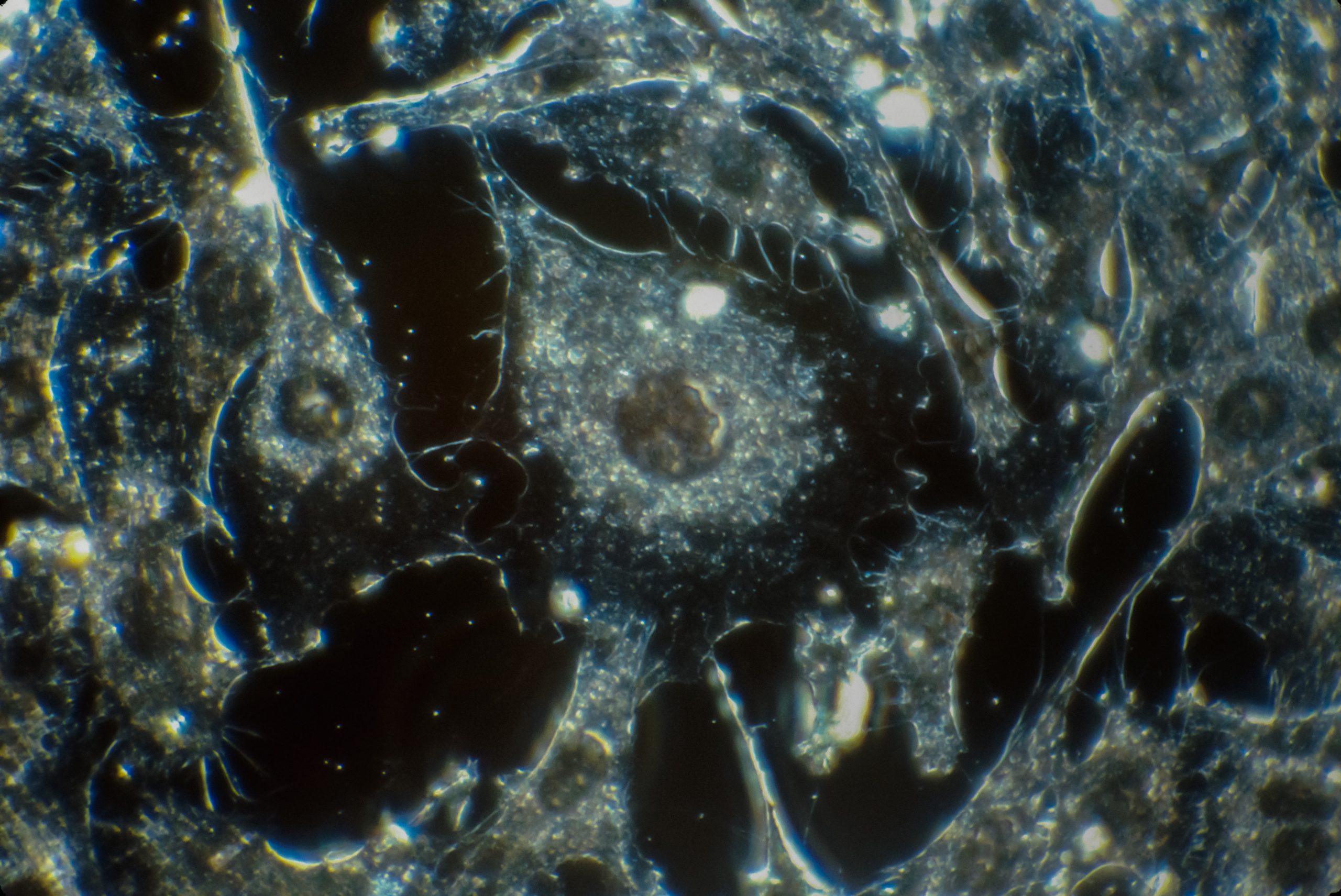
There are different sub-forms, which differ in their histologic composition. The most common gynecological sarcoma, at over 50%, is leiomyosarcoma of the uterus, the second most common is endometrial stromal sarcoma, which also occurs in the uterus. There are also many rare gynecological forms of sarcoma, such as liposarcoma or angiosarcoma. Although it is more of a disease that occurs at an older age, women of any age can be affected by this disease.
Diagnosis: How can a sarcoma be diagnosed?
Most sarcomas are diagnosed very late, as they often only cause symptoms when the tumor is in an advanced stage. For example, a sarcoma can cause pulmonary metastases, which then restrict lung function, i.e. cause shortness of breath. A symptom can also be that pain does not improve over time, but manifests itself over many weeks and even worsens, such as: B. in a sarcoma of the uterus. In rare cases, atypical bleeding during or after menstruation can also be a first symptom. If the sarcoma is located in the area of the ovary, the patient usually only feels symptoms at a very advanced stage. It is often pain or an increase in abdominal circumference that ultimately prompts the patient to see a doctor, who then diagnoses a sarcoma. A real early detection or preventive examination is therefore not possible with sarcomas, not even with a smear in the area of the uterus.
Therapy: How are sarcomas treated?
The treatment of gynecological sarcomas is interdisciplinary (including radiology, pathology, gynaecology, general surgery). It mainly depends on the tumor stage, the tissue type and the health and physical status of the patient. In an early tumor stage, surgery alone can be the only and sufficient treatment. In the case of certain risk factors such as distant metastases or tumor residues at the surgical margins, chemotherapy or radiation can be part of the so-called multimodal therapy strategy. In the case of advanced tumor stages with distant spread or in the event of recurrence, medication – usually chemotherapy or a targeted therapy strategy – is also used. The collective term “targeted therapy strategies” summarizes novel treatment approaches which, as the name suggests — in contrast to the broad effect (“cell division poison”) of classic chemotherapy — are used in a targeted manner against a single, specific structure. This can be an antibody or so-called “small molecules” that are so small that they can penetrate the sarcoma cell and affect cell metabolism there.
What does the prognosis of my disease depend on?
Unfortunately, a sarcoma is an aggressive form of tumor with a rather poor prognosis. Although many more women with gynecological sarcomas are surviving today than 30 years ago thanks to significantly improved surgical techniques, little progress has been made in recent decades. The rarity of the disease poses a major problem for the further development of therapy and thus the improvement of the prognosis. If you look at the example of breast cancer, the most common cancer in women, you can see that the prognosis has improved massively in recent decades. This made countless studies possible, in which several hundred thousand patients took part. As a result of this very intensive research activity, numerous new insights were gained. The field of sarcomas is only just beginning.
In principle, however, a cure is also possible for malignant tumors. The exact determination of the sarcoma subtype is important for the treatment. This depends on the tumor biological factors, which are described in particular by the tumor stage. An early-stage tumor has a very high chance of recovery, while a later-stage tumor with distant metastases is already present,
the chances of recovery are usually only small. The chances increase significantly if the sarcoma can be completely removed by surgery (with a border of healthy surrounding tissue, surgeons then speak of a tumor compartment). However, such an operation is not always possible. Even a successful operation does not necessarily guarantee a cure. In any case, sarcomas should be treated in specialized sarcoma centers.
The prognosis is influenced by many different factors. On the one hand, there are tumor-typical factors, such as B. the tumor size, the degree of differentiation of the cells and the tissue type, but on the other hand general factors also play a role, such as the physical condition of the patient, her age and the functional status of her organs (blood count, kidney values, kidney function, etc.).
Aftercare
After completion of the therapy, an individual medical aftercare plan should be discussed in cooperation with the attending physician. This is valid for the next five years, in accordance with the guidelines for gynecological oncology. Follow-up appointments are initially held about every three months. Later the examination
intervals become longer. As a rule, the aftercare appointments can be made on an outpatient basis with a specialist or in specialized clinics such as the Charité Women’s Clinic. The doctor in charge will constantly check whether the consequences of the therapy are leading to impairments and whether new cancer cells have formed so that they can be treated quickly if necessary. Here, too, the following applies: If a recurrence discovered early can be completely removed, the prognosis is good.
If you have any questions about sarcomas, you can also contact the cancer information service personally: on the free telephone number 0800 — 420 30 40 or by e‑mail to krebsinformationsdienst@dkfz.de.
Sources:
Gesund.bund.de — Sarkome
Verlässliche Informationen für Ihre Gesundheit
Deutsche Sarkomstiftung — sarkome.de
Informations- und Austausch-Plattform für Patienten, Angehörige, Mediziner, Forscher und andere Vertreter des Gesundheitssystems
Charité — Universitätsmedizin Berlin — https://frauenklinik.charite.de/
Sarkomerfahrene Mediziner und Sarkom-Zentrum